2nd International Conference on Non-invasive Cardiac Imaging, Nuclear Cardiology & Echocardiography
Amsterdam, Netherlands

Louis Peeters
Utrecht University, Netherlands
Title: Pathophysiology of Hypertensive Disorders of Pregnancy (HDPs): Current insights
Biography
Biography: Louis Peeters
Abstract
Introduction: Current management of HDPs is symptomatic intended to 1) prevent deterioration of unstable cardiovascular and renal functions, and 2) minimize the infant’s risk of permanent hypoxia/prematurity- related damage. Since ≈1980 our insight in the normal and abnormal cardiovascular and volume responses to normal and HDP-pregnancies has improved markedly, offering options to develop more causal and with it, probably more effective HDP management strategies.This lecture summarizes current insights in the mechanisms orchestrating maternal cardiovascular/volume responses to pregnancy, and with it, provides clues when and how these normal adaptations deteriorate allowing HDP to develop.
Normal cardiovascular adaptation: Within 10 days after embryo im- plantation, plasma osmolality (fig. 1) and arterial blood pressure [2] fall abruptly, probably echoing the hemodynamic effects of systemic vascular relaxation and associated fall in cardiac pre- and afterload. They trigger adaptations, which serve to secure circulatory functional integrity. Cardiac preload is restored by endocrine-induced plasma volume expansion along with the concomitant development of a more negative intrathoracic (suction) pressure. Cardiac afterload is restored by a rise in cardiac output (CO) via a baroreceptor-mediated rise in cardiovascular sympathetic tone. Preservation of the balance between cardiac pre- and afterload is pivotal for optimal cardiac function all through pregnancy (3, 4, 5).
Defective cardiovascular adaptation: Inherent to HDPs being defined by clinical signs is the heterogeneity of its preclinical pathophysiologic course. Nowadays, it is customary to differentiate between early- and late-onset HDP, primarily as they require a different clinical manage- ment. As a rule of thumb, physiologic adaptation to pregnancy deterio- rates when the balance between cardiac pre- and afterload becomes disturbed, necessitating a higher sympathetic contribution to the auto- nomic regulation of the circulatory function to preserve cardiovascular functional integrity, though, at the cost of the uteroplacental perfusion and with it, the growth of the placental functional capacity.
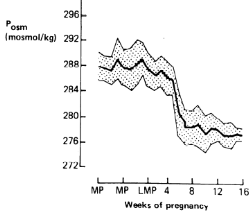
Figure 1: Weekly plasma osmolality (Posmol ± SD) before and during early pregnancy in 9 healthy pregnancies. MP and LMP indicate menstrual and last menstrual periods, respectively. (Adopted and modified from ref 1).
References:
- Davison JM et al, Plasma osmolality and urinary concentration and dilution during/after pregnancy. Brit J Obstet Gynaecol 1981;88:472.
- Spaanderman ME et al, The effect of pregnancy on the compliance of large arteries and veins in normal parous controls and formerly preeclamptics. Am J Obstet Gynecol 2000; 183: 1278.
- Valdes G et al. Challenges posed to the maternal circulation by preg- nancy (review). Integrated Blood Pressure Control 2011; 4: 45.
- Melchiorre K et al. Cardiac structure & function in normal pregnancy.Curr. Opin. Obstet. Gynaecol. 2012; 24: 413.
- Melchiorre K et al. Cardiac structure & function in normal pregnancy.Curr. Opin. Obstet. Gynaecol. 2012; 24: 413.Chung E et al. Pregnancy as a cardiac stress model. Cardiovasc. Res. 2014; 101: 561-570.