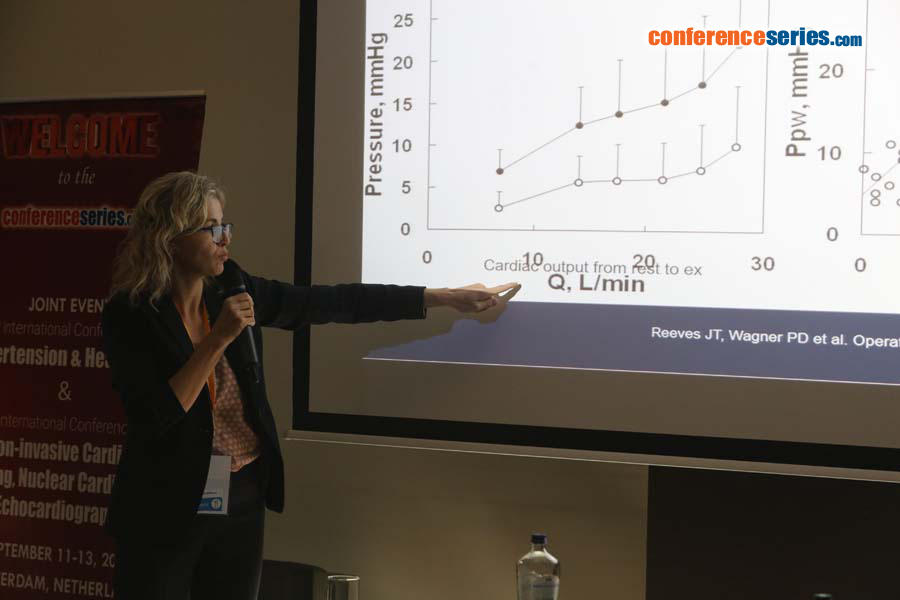
2nd International Conference on Non-invasive Cardiac Imaging, Nuclear Cardiology & Echocardiography
Amsterdam, Netherlands

Fabiola B Sozzi
University of Milan, Italy
Title: When and how to perform diastolic stress echocardiography?
Biography
Biography: Fabiola B Sozzi
Abstract
While echocardiographic grading of left ventricular diastolic dysfunction is used every day, the interactions between diastolic dysfunction grade at echocardiography and the hemodynamic abnormalities are still not completely clarified (1). Collectively, there is growing evidence that the diastolic stress test can provide important diagnostic findings that can be helpful in the management of patients presenting with dyspnea of an unclear etiology. Many patients present with exertional dyspnea and exercise intolerance, but have normal left ventricular filling pressures at rest. In these patients, it is important to evaluate filling pressure with exercise. Exercise can be performed using a supine bicycle or treadmill protocol. Alterantively dobutamine can be used, though its vasodilator as well as inotrope effect determine a very different hemodynamic response compared to that of exercise. We need to record mitral inflow by pulsed doppler echocardiography at the level of the mitral tips, mitral annular velocities by spectral doppler echocardiography, and tricuspid regurgitation jet by continuous-wave doppler at baseline and after the termination of exercise. Diastolic function parameters can be obtained after the assessment of regional wall motion abnormalities, especially when an exercise echocardiogram is performed for the evaluation of dyspnea. In patients with diastolic heart failure, left atrial pressure is increased, leading to an increase in mitral E velocity, whereas annular e’ velocity remains reduced given the limited preload effect on e’. Moreover, an increase in the pulmonary artery systolic pressure can be detected by the increase in peak velocity of the tricuspid regurgitation jet (2). On the other hand, in the absence of cardiac disease, e’ increases to a similar extent to the increase in mitral E velocity, and the normal E/e’ ratio essentially is unchanged with exercise (3). The concept of the diastolic stress test were introduced more than 10 years ago. Subsequently, exercise E/e’ ratio was validated against invasive measurements. Importantly, exercise septal E/e’ ratio was an important determinant of exercise capacity, and its decline with age was noted in a large series of patients referred for exercise echocardiography. Furthermore, a recent study showed the incremental prognostic value of exercise E/e’ ratio over clinical variables and exercise wall motion score index.
In conclusion, diastolic stress test has an interesting role in patients with heart failure and preserved ejection fraction that present symptoms during activity, normal ejection fraction and inconclusive diastolic function at rest.
References:
- Oh JK, Park SJ, Nagueh SF. Established and Novel Clinical Applications of Diastolic Function Assessment by Echocardiography. Circ Cardiovasc Imaging 2011;4:444-445
- Kane GC, Oh JK. Diastolic Stress Test for the Evaluation of Exertional Dyspnea. Curr Cardiol Rep 2012;14:359-365
- Ratanasit N, Karaketklang K, Chirakarnjanakorn S, Krittayaphong R, Jakrapanichakul D. Left atrial volume as an independent predictor of exercise capacity in patients with isolated diastolic dysfunction presented with exertional dyspnea. Cardiovascular Ultrasound 2014,12:19-26