Day 1 :
Keynote Forum
Michiel Voskuil
Universitair Medisch Centrum Utrecht, The Netherlands
Keynote: Renal denervation in 2017; A glimpse of hope
Time : 9:45- 10:45

Biography:
Abstract:
Keynote Forum
Peter J Blankestijn
University Medical Center Utrecht, The Netherlands
Keynote: Renal denervation: present situation and perspectives for the future
Time : 10:15-10:55

Biography:
Abstract:
Renal denervation has been introduced for the treatment of resistance hypertension. There is considerable theoretical and experimental evidence that renal denervation may be an effective antihypertensive treatment. Presently available clinical evidence in conflicting, but large randomized controlled trials are underway and first results will be presented later in 2017.
In this presentation the present status on safety and efficacy and considerations for the future of renal denervation in hypertensive patients will be discussed. It is now clear that poor medication adherence is a common finding is resistant hypertension patients. How this interacts with renal denervation will be addressed. Finally, possible other patient groups that may benefit of renal denervation are mentioned as well.
Keynote Forum
Boris Y Zaslavsky
Cleveland Diagnostics, USA
Keynote: Properties of membrane-less organelles and aqueous two-phase systems

Biography:
Boris Y Zaslavsky is a Bioanalytical Chemist. He graduated from Moscow State University in 1967, PhD in 1972; DSc in 1985 from USSR Academy of Sciences, Moscow, USSR. From 2012-present, he is a Chief Scientific Officer of Cleveland Diagnostics, Cleveland, OH, from 1997-present, he is a Vice President, Director of Research and Cofounder of Analiza, Inc., Cleveland, OH. He has over 180 publications in peer-reviewed journals, 1 monograph, over 10 USA and international patents issued. His research interests are: Clinical proteomics, role of water in biology, and aqueous two-phase systems.
Abstract:
Coordination of numerous cellular biochemical reactions in space and time is achieved by compartmentalization. In addition to intracellular membranes acting as physical barriers for several cellular organelles there is a multitude of membrane-less organelles formed by liquid-liquid phase separation. The principles governing phase separation and functions of such organelles in vivo are poorly understood as of now. However, the much better studied aqueous two-phase systems formed by two polymers may serve as a model of membrane-less organelles. Such systems originate from polymer influence on the solvent properties of water. The phase forming polymers may include proteins and polysaccharides. The differences between solvent features of aqueous media in the two phases may be quantified and manipulated by polymers’ concentrations and additives of inorganic salts or small organic compounds, such as sucrose, sorbitol, etc. The differences between electrostatic properties of the phases as well as those between solvent features may be quantified using partitioning of homologous series of charged compounds and solvatochromic dyes as molecular probes for the solvent dipolarity/polarizability, solvent H-bond donor acidity, and solvent H-bond acceptor basicity. The differences between solvent features and electrostatic properties of the phases govern unequal distribution of proteins and other natural compounds in aqueous two phase systems and in membrane-less organelles. This solvent-driven partitioning, and not the “normal” protein-protein interactions, might cause enrichment of some proteins within the membrane-less organelles. It will be shown that proteins may influence solvent features of water and their effects are similar or exceeding those displayed by common macromolecular crowding agents and organic osmolytes. It is suggested that the effects of proteins on the solvent features of aqueous media may regulate the phase separation in vivo.
- Sessions
Location: Amsterdam, Netherlands
Session Introduction
Fabiola B Sozzi
University of Milan, Italy
Title: When and how to perform diastolic stress echocardiography?
Time : 11:10-11:40

Biography:
Fabiola Sozzi works as a staff cardiologist at the University Hospital Policlinico of Milan, Italy, with high-specialization nomination. She has high skills in multimodality imaging of heart disease using echocardiography integrated with cardiac magnetic resonance imaging, cardiac computed tomography and nuclear. She also works in the acute clinical setting treating acute cardiac syndromes. She gained a high expertise in echocardiography at the Thoraxcentre of Rotterdam (NL), where she defended the PhD thesis on stress cardiac imaging under the supervision of Professor J. Roelandt. She is Visiting Professor at the University of Milan where she leads several research projects and teaches at the Faculty of Medicine and School of Specialization of Cardiology. She is author of 70 papers published in indexed peer-reviewed international journals and reviewer of several medical international journals.
Abstract:
While echocardiographic grading of left ventricular diastolic dysfunction is used every day, the interactions between diastolic dysfunction grade at echocardiography and the hemodynamic abnormalities are still not completely clarified (1). Collectively, there is growing evidence that the diastolic stress test can provide important diagnostic findings that can be helpful in the management of patients presenting with dyspnea of an unclear etiology. Many patients present with exertional dyspnea and exercise intolerance, but have normal left ventricular filling pressures at rest. In these patients, it is important to evaluate filling pressure with exercise. Exercise can be performed using a supine bicycle or treadmill protocol. Alterantively dobutamine can be used, though its vasodilator as well as inotrope effect determine a very different hemodynamic response compared to that of exercise. We need to record mitral inflow by pulsed doppler echocardiography at the level of the mitral tips, mitral annular velocities by spectral doppler echocardiography, and tricuspid regurgitation jet by continuous-wave doppler at baseline and after the termination of exercise. Diastolic function parameters can be obtained after the assessment of regional wall motion abnormalities, especially when an exercise echocardiogram is performed for the evaluation of dyspnea. In patients with diastolic heart failure, left atrial pressure is increased, leading to an increase in mitral E velocity, whereas annular e’ velocity remains reduced given the limited preload effect on e’. Moreover, an increase in the pulmonary artery systolic pressure can be detected by the increase in peak velocity of the tricuspid regurgitation jet (2). On the other hand, in the absence of cardiac disease, e’ increases to a similar extent to the increase in mitral E velocity, and the normal E/e’ ratio essentially is unchanged with exercise (3). The concept of the diastolic stress test were introduced more than 10 years ago. Subsequently, exercise E/e’ ratio was validated against invasive measurements. Importantly, exercise septal E/e’ ratio was an important determinant of exercise capacity, and its decline with age was noted in a large series of patients referred for exercise echocardiography. Furthermore, a recent study showed the incremental prognostic value of exercise E/e’ ratio over clinical variables and exercise wall motion score index.
In conclusion, diastolic stress test has an interesting role in patients with heart failure and preserved ejection fraction that present symptoms during activity, normal ejection fraction and inconclusive diastolic function at rest.
References:
- Oh JK, Park SJ, Nagueh SF. Established and Novel Clinical Applications of Diastolic Function Assessment by Echocardiography. Circ Cardiovasc Imaging 2011;4:444-445
- Kane GC, Oh JK. Diastolic Stress Test for the Evaluation of Exertional Dyspnea. Curr Cardiol Rep 2012;14:359-365
- Ratanasit N, Karaketklang K, Chirakarnjanakorn S, Krittayaphong R, Jakrapanichakul D. Left atrial volume as an independent predictor of exercise capacity in patients with isolated diastolic dysfunction presented with exertional dyspnea. Cardiovascular Ultrasound 2014,12:19-26
Vladimir A.Mikhaylov
Eternity Medicine Institute, Dubai
Title: Newly discovered way of the function of cardio-vascular system and the latest theory of the development of hypertension and other cardiovascular diseases
Time : 11:40-12:10

Biography:
1982 - After receiving his medical degree from the Ryazan medical institute named after I.P. Pavlov (M.D.) protected a degree of Ph.D. (Formation dublical anastomosis in surgery of intestinum and pancreas. 1994 - received a degree Sci.D. in National center of laser medicine in Moscow (Use of low- level of laser radiation in treatment of oncology diseases. 1997 - Ðead of Moscow Scientific-Practical Center of laser Medicine. 1999 - selected in Board of directors (EMLA), direction – oncology and angiology in Vienna, Austria. 2001- President of the VIIIth Congress of European Medical Laser Association (EMLA), Moscow, Russia. The member of international editorial board of the “Laser Therapy”. 2009 - Has been recognized as an International Medical Laser Specialist at class: Hon-IMeLas, Number: H-0017, Congress ISLSM, WFSLMS, Tokyo, November 27, 2009. 2013 - Physician Contract with Eternity Medicine Institute, Dubai, Social activity. 2015 - Award winner - Ming Chien Kao Awards 2015 (For publishing article- . Use of intravenous laser blood irradiation (ilbi) at 630-640 nm to prevent vascular diseases and to increase life expectancy. Laser Therapy, vol 24(2015), No.1, p.15-26).
Abstract:
Statement of the Problem: It is known that the power of the heart alone is about 3.3 W, and the length of the vessels is about 100,000 km. It made us doubt that with this power the heart can deliver blood to the capillary bed. Effects on the vascular wall of various modes of laser radiation (wavelength of 630-640 nm.) showed that if continuous radiation did not affect the parameters of blood pressure, frequency regimes had an impact. This leads us to the idea that the root cause of the development of different cardiovascular diseases is the system disturbance of the activity of the vascular pump leads to the increase of intra vascular pressure and the emergence of the hypertensive illness and the coronary heart disease.
Theoretical Orientation: To confirm this idea that the main role in
he delivery of blood to tissues primarily played by the vessels and not the heart, we conducted the following studies: 1. Built a new mathematical model . 2. Changed features of the anatomical structure of different types of arteries. 3. Explained how the synchronization of the heart and blood vessels transporting blood to the tissues.
Conclusion & Significance: The main role in transportation of blood to the capillary bed play a artery, the power of the heart is only 0,49 -0,027% of the power needed to transport blood to the capillary bed. The vascular pump is regulated by the frequency of contractions of the heart muscle and is tightly synchronized with the work of the heart. The rapid spread of the pulse wave creating a suction effect. Following the reduction of the vessel wall, the blood just drawn from the aorta and large arteries to the smaller vessels down to the capillary bed. Systematic irregularities in the vascular pump are the starting point in the development of hypertension. These illnesses may be both local and systemic, depending on the size and location of pathological changes in the vascular wall.
Recommendations: It is necessary to conduct further studies to confirm the mechanisms of development of hypertension.
References:
- McDonald, D.A.: Blood flow in arteries. Second ed. London: Arnold 1974.
- GUYTON, A.C., YOUNG, D.B. (Eds): Cardiovascular Physiology III, Vol. 18, Baltimore: University Park Press, 1979.
- Mikhaylov V.A., (2007) Intravenous laser blood irradiation, Greece, 2007, 102 p.
- Mikhaylov V.A., (2015), Use of intravenous laser blood irradiation (ilbi) at 630-640 nm to prevent vascular diseases and to increase life expectancy. Laser Therapy, vol 24, No.1, p.15-26
- Mikhaylov V.A., (2016) Ming Chien Kao Awards 2015, Laser Therapy, mar 2016, vol. 25, No.1, p.9-10.
Valéria Paula S. Fazan
University of São Paulo ,Brazil
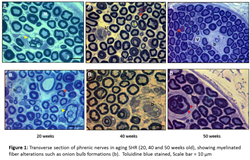
Title: Evidence of a hypertensive peripheral neuropathy in an experimental model of hypertension in rats
Time : 14:10-14:40

Biography:
Valéria Paula Sassoli Fazan graduated in the School of Medicine of Ribeirão Preto, University of São Paulo, in 1991 and attended the Neurosurgery Residency Program at the same University. Obtained the M.S. Degree in Morphology in 1995 and Ph.D. Degree in Neurology in 1999, both in the the School of Medicine of Ribeirão Preto. Currently is an Associate Professor in the Department of Surgery and Anatomy and Manager of the Microsopy and Morphometry Laboratory at the Experimental Surgery Center in the School of Medicine of Ribeirão Preto, University of São Paulo. Proficient with a wide-range of light and electron microscopy techniques including specimen preparation and handling, vacuum evaporation and autoradiography, light microscopy including brightfield, darkfield, phase, fluorescence and transmission electron microscopy including brightfield and darkfield. Expert in neuroscience, particularly in the fields of peripheral nerves and experimental models of neuropathies, digital image processing and analysis, stereology and morphometry.
Abstract:
Statement of the Problem: Spontaneously hypertensive rats (SHR), first inbred from Wistar Kyoto rats (WKY), are considered a good experimental model of human essential hypertension. Hypertension is a main risk factor for stroke and vascular dementia and may cause important changes to the cerebrovascular tree, turning the brain more susceptible to infarcts, microaneurysms and ischemia. In spite of the well documented influence of hypertension on the brain, data on the sensitivity of peripheral nerves in hypertension is scarce. The purpose of this study was to investigate the alterations on the morphology and morphometric data on sural, phrenic and vagus nerves of adult SHR, with well-established hypertension.
Methodology & Theoretical Orientation: Male and female SHR and normotensive WKY rats aged 20 weeks (N = 6 in each group) were investigated. After arterial pressure and heart rate recordings in anesthetized animals, right and left sural nerves were removed and prepared for epoxy resin embedding and light microscopy. Morphometric analysis was performed with the aid of computer software, and took into consideration the fascicle area and diameter, as well as myelinated fiber number, density, area and diameter.
Findings: Significant differences were observed for the myelinated fiber number and density, comparing different genders of WKY and SHR in all nerves. Also, significant differences for the morphological (thickening of the endoneural blood vessel walls and lumen reduction) and morphometric (myelinated fibers diameter and G ratio) parameters of myelinated fibers were identified.
Conclusion & Significance: Morphological exam of the myelinated fibers suggested the presence of a neuropathy due to hypertension in both SHR genders. These results indicate that hypertension altered important morphometric parameters related to nerve conduction in hypertensive animals. Moreover the comparison between males and females of WKY and SHR showed that the morphological and morphometric alterations due to hypertension are not gender related.
References:
- Da Silva GA, Mendes VA, Genari AB, Castania JA, Salgado HC, Fazan VPS (2016), Recurrent laryngeal nerve alterations in developing spontaneously hypertensive rats. Laryngoscope 126(1):E40-7
- Sanada LS, Tavares MR, Sato KL, Ferreira R da S, Neubern MC, Castania JA, Salgado HC, Fazan VPS (2015) Association of chronic diabetes and hypertension in sural nerve morphometry: an experimental study. Diabetol Metab Syndr 7:9.
- Oliveira FS, Nessler RA, Castania JA, Salgado HC, Fazan VPS (2013), Ultra structural and morphometric alterations in the aortic depressor nerve of rats due to long-term experimental diabetes: effects of insulin treatment. Brain Res 1491:197-203.
- Sanada LS, da Rocha Kalil AL, Tavares MR, Neubern MC, Salgado HC, Fazan VPS (2012), Sural nerve involvement in experimental hypertension: morphology and morphometry in male and female normotensive Wistar-Kyoto (WKY) and spontaneously hypertensive rats (SHR). BMC Neurosci 13:24
- Rodrigues AR, Ferreira RS, Salgado HC, Fazan VPS (2011) Morphometric analysis of the phrenic nerve in male and female Wistar-Kyoto (WKY) and spontaneously hypertensive rats (SHR). Braz J Med Biol Res 44(6): 583-591.
Nilda Gladys Espinola-Zavaleta
National Institute of Cardiology Ignacio Chavez, Mexico
Title: The Polymorphism LDB3 rs (45618633), TAZ rs (104894941), LMNA (rs28928903), DTNA (rs7243528) and TNNT2 G/T (rs 2365652) and its associate with non compacted cardiomyopathy in Mexican Mestizo family
Time : 14:40-15:10

Biography:
Nilda Espinola-Zavaleta is a Cardiologists and echocardiographist of the National Institute of Cardiology “Ignacio Chavez” in Mexico City. She is a national researcher and her work is focused in pulmonary hypertension, right venricular function, congenital heart disease, ischemic heart disease, valvular heart disease, cardiomyopathies and new techniques of echocardiography.
Abstract:
Background: Noncompacted cardiomyopathy (NCC) has been attributed to the mutation in multiple genes leading to interruption in the endomyocardial compaction process. In the affected families, associations with mutations without T gene of cardiac troponin (TNNT2) and of the genes LDB3, MYH7 and ACTC, dystrobrevin (DTNA) and tafazzin (TAZ) in some with recessive inheritance and others of dominant type were found.
Objective: The objective of this work was to identify gene variants that participated in the development of NCC in a Mexican mestizo family.
Material and methods: A total of 36 (85.7%) individuals from a family of 42 members were studied. All patients underwent clinical history, transthoracic echocardiography (according to the criteria of Jenni et al) and the polymorphisms: LDB3, TAZ, LMNA, DTNA and TNNT2 G/T were obtained from whole blood through a commercial kit (WizardGenomic DNA Isolation Kit: Promega, Wisconsin).
Results: The NCC was present in 36.1% of the patients. Seven are first-generation relatives, of whom 6 presented NCC. Thirty-three second-generation relatives of whom 6 patients were positive for the disease and 2 third-generation individuals without NCC. When evaluating those with NCC vs those without NCC, differences in diastolic diameter, systolic diameter, left atrium size, left ventricuar ejection fraction, and pulmonary artery systolic pressure were found. The 100% of patients with NCC presented the A and C alleles in the polymorphisms (rs 45618633) of the LDB3 gene and (rs 104894941) of the TAZ gene. While, for the GG and TT genotype in LMNA polymorphisms (rs 28928903) and DTNA (rs 7243528) no patients with NCC were found. At follow-up, 4/13 patients with ventricular noncompaction died.
Conclusions: 36.1% of patients in the Mexican mestizo family studied developed NCC and 100% presented the A and C alleles in the polymorphisms (rs 45618633) of the LDB3 gene and (rs 104894941) of the TAZ gene. At follow-up, 30.7% of patients with NCC died.
References:
1.Maron BJ, Towbin JA, Thiene G, Antzelevitch et al. Contemporary definitions and classication of the cardiomyopathies: an American Heart Association Scientific Statement from the Council on Clinical Cardiology, Heart Failure and Transplantation Committee; Quality of Care and Outcomes Research and Functional Genomics and Translational Biology Interdisciplinary Working Groups; and Council on Epidemiology and Prevention. Circulation. 2006;113:1807-16.
2. Monserrat L, Hermida-Prieto M, Fernandez X, Rodriguez I, Dumont C, Cazon L et al. Mutation in the alpha-cardiac actin gene associated with apical hypertrophic cardiomyopathy left ventricular non-compaction, and septal defects. Eur Heart J 2007;28:1953–1961.
Patricia Hidalgo M
San Ignacio-Pontificia Universidad Javeriana, Colombia
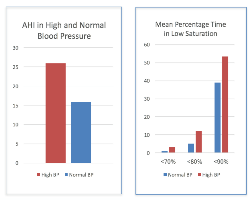
Title: Associations of time of oxygen saturation below 90% with apnea-hypopnea index (AHI) and the presence of high blood pressure (HBP) at 2640masl
Time : 16:15-16:45

Biography:
Alvaro Ruiz and Patricia Hidalgo have their expertise in internal medicine, clinical epidemiology and sleep disorders at high altitudes. They have built their way of focusing after years of experience in medical practice, research and teaching both in hospital and education institutions. They are research seed leaders and have population based published papers and also health guidelines.
Abstract:
Statement of the Problem: Chronic hypoxia causes marked activation of the sympathetic nervous system and elicits systemic oxidative stress. Time of oxygen desaturation during sleep might be a risk factor for HBP and even more at higher altitudes. The purpose of this study was to describe whether the percentage of time of oxygen desaturation during a sleep study was associated with the presence of HBP or with higher AHI.
Methodology & Theoretical Orientation: We performed a descriptive study among 648 patients attending the sleep lab. Sleep studies were interpreted according to the AASM parameters and the percentage of time of oxygen saturation below 90(TS90), 80(TS80) and 70(TS70) were calculated. The presence of HBP was documented by either by patient report, recorded medication or direct measurement of blood pressure levels at the beginning and at the end of the sleep study.
Findings: HBP was associated with higher AHI (95% confidence interval [95% CI]: 25.9(23.40, 28.55) compared to no HBP (95% confidence interval [95% CI]: 15.9(13.97, 17.98), P-value <0.0001. Being male was associated with higher AHI. TS90 were higher in patients with HBP: 58.4(95%CI =52.64, 64.29) compared to those without HBP: 40.2(95% CI= 36.52, 44.05), P-value <0.0001. The effect estimate attenuated when TS below 80 or 70 was taken into account but remained significant (P-value = 0.0012).
Conclusion & Significance: Low levels of oxygen saturation during sleep were associated with higher AHIs. Additional adjustment for lower oxygen saturation levels reduced the effect size of the association but remained significant. Further studies are needed to replicate these findings and to examine mechanisms underlying the observed association and the long-term consequences in HBP development and treatment.
References:
- Lu W, Kang J, Hu K, Tang S, et al., The role of the Nox4-derived ROS- mediated RhoA/Rho kinase pathway in rat hypertension induced by chronic intermittent hypoxia. Sleep and Breathing. Jan 2017:1-11.
- Calbet J. Chronic hypoxia increases blood pressure and noradrenaline spillover in healthy humans. Physiol.2003; 551.1, pp. 379–386.
- Almeida G, Trombetta I, Cepeda F, Hatanaka E, et al., (2017), The role of acute intermittent hypoxia in neutrophil-generated superoxide, sympathovagal balance, and vascular function in healthy subjects, Frontiers in Physiology, 2017; 8(1), Article number 4.
- Lang M, Faini A, Caravita S, Bilo G, et al., (2016), Blood pressure response to six-minute walk test in hypertensive subjects exposed to high altitude: Effects antihypertensive combination treatment International Journal of Cardiology., 219: 27-32.
- Tremblay j, Boulet L, Tymko M, Foster G., (2016), Intermittent hypoxia and arterial blood pressure control in humans: Role of the peripheral vasculature and carotid baroreflex, American Journal of Physiology-Heart and Circulatory Physiology. 311(3):699-706.
Amar Mohanrao Taksande
Jawaharlal Nehru Medical College, India
Title: Evaluation of Neonatal echocardiography in the neonatal intensive care unit
Time : 16:45-17:15

Biography:
Amar Taksande is presently working as Professor in Dept. of Pediatrics, at Jawaharlal Nehru Medical College (JNMC), DMIMS, Sawangi. He completed his residency at Mahatma Gandhi Institute of Medical Sciences (MGIMS) Medical College, Sevagram where he also worked as Associate Professor in the Pediatric Department. He got Fellowship in Pediatric Cardiology at Innova children heart hospital, Hyderabad. He received an award of Visiting Fellowship by Royal College of Pediatric and Child Health (RCPCH), United Kingdom. He has published over 135 papers in national and inter-national journals and is author of several paediatrics titles. He is life member of Indian Academy of Pediatrics, Pediatric Cardiology Society of India and several other medical organizations. He is also a peer reviewer of international Journals like congenital heart disease, Journal of Pediatrics, Journal of Pediatric Infectious disease etc.
Abstract:
Introduction:
Congenital Heart Disease (CHD) is the most common congenital problem that accounts for up to 25% of all congenital malformations that present in the neonatal period and is leading cause of neonatal and infant mortality. Echocardiography is an investigation that is currently being used in many neonatal intensive care units (NICU) to evaluate disease progress, assist in procedural interventions, assess the functional or structural defects of the critically ill neonates at the bedside.
Objective:
To evaluate the role of neonatal echocardiographic examination in the clinical management of the sick neonate in NICU.
Material and Methods:
Study was conducted in the NICU of Paediatric department of a Rural Medical College in Central India over a period of 2 years. Information about all echocardiograms performed in the neonatal unit was collected prospectively. Indications for performing echocardiography, echocardiographic findings, and any resulting changes in clinical management were determined.
Results:
A total of 231 echocardiograms were performed in 182 neonates. Echocardiography identified 74 neonates with a structural cardiac abnormality. Patent oval foramen and hemodynamically nonsignificant patent arterial duct (20%) and physiologic pulmonary artery stenosis (2%) were categorized as normal structural group. In addition, 11 neonates were found to have an important functional abnormality. Murmurs (55%) followed by extracardiac anomalies and dysmorphic features (32%) were the most common clinical indications for requesting an echocardiogram. Echocardiography prompted a specific change in clinical management in 72% neonates. Murmur in our critically ill neonates has been associated with a higher incidence of cardiac disease.
Conclusion:
Bedside echocardiography had provided crucial information and accurate decision makings that was not apparent on clinical assessment. Hence, echocardiography is an important tool for diagnosis of cardiac abnormalities that can influence the management and outcome of the sick newborn in the intensive care unit.
- Young Research Forum
Location: Amsterdam, Netherlands
Session Introduction
Ayush Shrivastava
Jawaharlal Nehru Medical College, India
Title: Study of tissue doppler imaging (TDI) for myocardial velocity in Sickle-Cell disease children
Time : 17:15-17:30

Biography:
I Ayush Shrivastava belong to Bhopal, Madhya Pradesh, India had done undergraduate from People’s College of Medical Science and research center, Bhanpur, Bhopal and is doing residency in Paediatrics from Jawaharlal Nehru Medical College, Sawangi, Wardha, Maharashtra.
Abstract:
Background:
Sickle-cell disease (SCD) is an inherited hemoglobin childhood disorder, frequently complicated by pulmonary hypertension and cardiac involvement. Tissue doppler imaging is the simple indices for the assessment of the cardiac function.
Aim:
To evaluate cardiac function by means of echocardiography in SCD children.
Study Design: Case control study
Methods:
30 children with SCD were compared with 30 age-matched healthy controls. Myocardial wall motion velocities at the lateral mitral annulus and the junction between the medial mitral annulus and the interventricular septum were assessed during systole (Sa), early diastole (Ea), and late diastole (Aa) through a four-chamber view using pulsed doppler echocardiography. The ejection fraction and shortening fraction were also estimated.
Results:
The early diastolic trans-tricuspid peak flow velocity was greater in the SCA patients than in the controls. Assessment of the lateral mitral and tricuspid annulus peak velocities by pulsed TDI showed that the patients had significantly greater systolic, and early and late diastolic velocities than the controls. The left ventricular diameter, interventricular septum diameter, and posterior wall diameter were statistically significantly greater in the SCD children compared with the control group, whereas there was no difference in ejection fraction. There was a significant difference in Sa(m) wave velocity between the two groups (p < 0.042).
Conclusion:
SCD in children results in a dilated heart with increase in left ventricular dimensions. TDI appears to be more sensitive in the early detection of myocardial dysfunction in SCD children.
Shreyas Rajendra Borkar
Jawaharlal Nehru Medical College, India
Title: Study of myocardial function assessment by tissue doppler imaging in neonates
Time : 17:30-17:45

Biography:
I, Dr. Shreyas Borkar completed my MBBS from Goverment Medical College, Nagpur under MUHS University, Nashik. I currently pursuing my post-graduation in Department of Pediatrics in JNMC, Sawangi Meghe, Wardha, Maharashtra, India.
Abstract:
Background: In both term and premature neonates, changes in the systolic and diastolic function of the left ventricle (LV) and right ventricle (RV) reflect the degree of neonatal myocardial immaturity and the co-existence of foetal circulation as well as the presence of concurrent diseases.
Aim: To measure the ventricular myocardial velocities using tissue doppler imaging (TDI) in the neonates.
Study Design: Prospective observational study
Material and Methods: Left and right ventricular peak systolic (S'), early diastolic (E') and late diastolic (A') myocardial velocities were measured using TDI alongside standard echocardiography. E/E' ratio was calculated for both ventricles. 20 neonates were prospectively recruited into two groups: Term (n=20) and preterm (<37 weeks, n=20)
Results: The diastolic myocardial velocities recorded in the RV were higher than those in the LV. Myocardial velocities increased in term child as compared to preterm child. Left E/E' ratio was higher than right in each group.
Conclusions: In neonates, the diastolic and systolic function recorded in the RV was better than that in the LV. Also, TDI is feasible in preterm neonates and enables the acquisition of myocardial velocities.
Mrudul Kumar
Jawaharlal Nehru Medical College, India
Title: Tissue Doppler Imaging (TDI) for evaluation of cardiac functions in infants of diabetic mothers (IDM)
Time : 17:45-18:00

Biography:
I Mrudul Kumar, completed by MBBS from Bhaskar Medical College and General hospital, Hyderabad, NTR University of Health Sciences. I am currently pursuing my post-graduation in the Department of Paediatrics (Second Year), from Jawaharlal Nehru Medical College, Datta Meghe Institute of Medical Sciences, Sawangi (Meghe), Wardha, Maharashtra.
Abstract:
Introduction: Congenital anomalies occur more commonly in infants born to diabetic mothers, and cardiac defects predominate. Infant of diabetic mothers often develop respiratory problems which need to be differentiated from the cardiovascular problems. Transient cardiac hypertrophy occurs in infants of diabetic mothers.
Aim: To evaluate the cardiac functions by using tissue doppler echocardiography in IDM.
Study Design: Case-Control Study
Material and Methods: Right and left ventricle systolic and diastolic functions of 15 term IDM and 15 healthy term newborns (control) were examined using TDI. Systolic (S'), early diastolic (E'), and late diastolic (A') TDI velocities were measured at the mitral valve (MV) annulus, basal interventricular septum (IVS), and tricuspid valve (TV) annulus. Demographic, perinatal, and echocardiographic variables were compared between IDM and control groups.
Results: IDMs groups had significantly greater birth weight, lower gestational age, older maternal age, and higher incidence of maternal obesity and hypertension than controls (p < 0.001). The septum was found to be thick in 5 (33.33%) of the IDM. Both the left and right ventricle myocardial velocities were found to be lower in the IDMs compared to the control group. Em/Am ratio was found to be less than one only in IDMs in the left ventricle in contrast to the control group.
Conclusion: Tissue Doppler Imaging demonstrated that IVS in IDM disrupt the diastolic function of both ventricles.
Toan Pham
Auckland Bio engineering Institute, New Zealand
Title: Right heart failure: Consequences for the mechanical efficiency of left-and rightventricular trabeculae from pulmonary hypertensive rats
Time : 18:00-18:15

Biography:
Toan Pham is doing research, which focused on the energetics and mechanisms of the progression from hypertrophy to heart failure. He is using different techniques of measuring cardiac efficiency: Microcalorimetry on trabeculae and Respirometry on mitochondrial functions.
Abstract:
An increase in pulmonary arterial pressure increases the load on the right ventricle (RV). With time, progressive pulmonary arterial hypertension (PAH) results in RV hypertrophy, leading ultimately to right-heart failure. In contrast, PAH reduces the passive filling pressure in the left ventricle (LV). This reduces the LV workload, thereby resulting in LV atrophy. Does the structural deformation of the ventricles in right-heart failure affect their mechanoenergetic performance? To address thisquestion, we used the PAH rat induced by a single injection of monocrotaline (MCT) (60 mg/kg) as our experimental model of right-heart failure. Six weeks after MCT injection, the hearts showed signs of right hypertrophy (indexed by increased free wall thickness) and left atrophy. Trabeculae tissue isolated from both ventricles of ‘Control’ and ‘PAH’ rats were mounted in our work-loop calorimeter, and subjected to stress-length work-loops over a wide range of afterloads while contracting at 5 Hz at 37 °C – a protocol designed to mimic the pressure-volume work of the heart. By simultaneously measuring heat production, mechanical efficiency was calculated as the ratio of work output to change of enthalpy (the sum of work and heat). The trabeculae were then required to undergo a preshortening protocol in which isometric force and heat output were measured as functions of muscle length. In right-heart failure secondary to pulmonary hypertension, RV trabeculae show a decrease in myocardial mechanical efficiency correlated with their lower stress-length work performance. The higher activation heat (ordinate of the heat-stress relationship) observed in RV trabeculae from the PAH group reflects an increased energy cost of Ca2+ cycling during contraction. In contrast, LV trabeculae from PAH group sustain normal energy efficiency over a wide range of afterloads.
- Workshop
Location: Amsterdam, Netherlands
Session Introduction
Hossein Tabriziani
Loma Linda University, USA
Title: Hypertension & cardiovascular disease after kidney transplantation
Time : 12:10-13:10

Biography:
Hossein Tabriziani has earned his MD with honors from Iran University of Medical Sciences (IUMS). He finished his Internal Medicine residency at St. Barnabas Hospital, Weill Cornell Medical College in New York. With passion for education and Transplantation, he accepted the fellowship in Nehrology and Hypertension at Georgetown University in Washington, DC and continued his education at University of California San Francisco (UCSF) with a Transplant Nephrology fellowship. He was appointed at the Medical director of Pancreas Transplantation at Westchester Medical Center, New York Medical college before moving to Loma Linda University in California to serve as an Assistant Professor of Medicine in Nephrology / Transplant division. He is an active member of American Society of Nephrology and American society of Transplantation. His interests are in Hypertension and Oxidative Stress in patients with chronic kidney disease and transplantation.
Abstract:
The incidence of end stage renal disease (ESRD) continues to rise in the United States. By the year 2030, the number of patients with ESRD is projected to exceed 2.2 million. This is more than five times the current prevalence.
During the past decade, kidney transplantation has increasingly been recognized as the treatment of choice for medically suitable patients with ESRD. As well as improving quality of life, successful transplantation confers major benefits by improving morbidity and mortality of ESRD patients who receive kidney transplant over those who undergo renal replacement therapy (RRT). Cardiovascular (CV) risk reduction remains the leading cause of this improvement, although both modalities provide compatible fluid balance and glomerular filtration.
As the Uited States Renal Data System (USRDS) shows, mortality is improved significantly for ESRD patients who received renal transplantation as compared to those with RRT.
Oxidative stress plays a key role in the pathophysiological process of uremia and its complications, particularly in cardiovascular disease. The level of oxidative stress markers is known to increase as Chronic Kidney Disease (CKD) progresses and correlates significantly with level of renal function.
Successful kidney transplantation, results in near normalization of the antioxidant status and lipid metabolism by eliminating free radicals despite the surge of oxidative stress caused by the surgical procedure and ischemic injury to the organ during the operation. This success is associated with both improved renal function, reduced cardiovascular complications, and overall improved morbidity and mortality.
Fabiola B Sozzi
University of Milan, Italy
Title: Unexplained dyspnea and diastolic function
Time : 15:10-16:00

Biography:
Fabiola Sozzi works as a staff cardiologist at the University Hospital Policlinico of Milan, Italy, with high-specialization nomination. She has high skills in multimodality imaging of heart disease using echocardiography integrated with cardiac magnetic resonance imaging, cardiac computed tomography and nuclear. She also works in the acute clinical setting treating acute cardiac syndromes. She gained a high expertise in echocardiography at the Thoraxcentre of Rotterdam (NL), where she defended the PhD thesis on stress cardiac imaging under the supervision of Professor J. Roelandt. She is Visiting Professor at the University of Milan where she leads several research projects and teaches at the Faculty of Medicine and School of Specialization of Cardiology. She is author of 70 papers published in indexed peer-reviewed international journals and reviewer of several medical international journals.
Abstract:
Chronic dyspnea is associated with a variety of diseases and is also a major symptom of heart failure (HF). The differential diagnosis of dyspnea is a daily routine in every cardiology practice. Approximately one-half of patients with HF have a preserved ejection fraction (HFpEF). Diagnosis of HFpEF is challenging and relies largely on demonstration of elevated cardiac filling pressures represented by the pulmonary capillary wedge pressure (1). The American College of Cardiology Foundation/American Heart Association guidelines define HFpEF as clinical signs and symptoms of HF, preserved ejection fraction, and no other obvious explanation for symptoms. This scheme works well for patients with a high likelihood of disease on the basis of clinical indicators of congestion. To address the patients without overt congestion, more recent guideline statements from the European Society of Cardiology (ESC) and American Society of Echocardiography/European Association
of Cardiovascular Imaging (ASE/EACVI) [2] require objective evidence of high left ventricular filling pressures. Elevated left ventricular filling pressure is a cardinal feature of HfpEF and can be clinically demonstrated by elevations in plasma natriuretic peptide levels. The ratio of transmitral E to mitral annular e' velocities (E/e') at doppler echocardiography has been proposed as a non-invasive measure of left ventricular filling pressure and endorsed by professional guidelines as a surrogate parameter of invasive left ventricular filling pressure in the diagnostic work-up of HFpEF. The diagnosis of HFpEF is straightforward when patients are acutely decompensated. To make matters more complex, many patients with HFpEF display normal left ventricular filling pressures at rest, with abnormalities that develop during stresses like exercise (3). Invasive hemodynamic exercise testing has emerged as the gold standard to diagnose or exclude HFpEF in patients with exertional dyspnea of unclear etiology, but cost, risk, and the requirement for specialized training and equipment may limit its broad application in practice and in clinical trials. Therefore, doppler echocardiography plays a central role in the non-invasive evaluation and grading of diastolic dysfunction.
References:
- Nagueh SF, Appleton CP, Gillebert TC, Marino PN, Oh JK, Smiseth OA, Waggoner AD, Flachskampf FA, Pellikka PA, Evangelisa A. Recommendations for the evaluation of left ventricular diastolic function by echocardiography. Eur J Echocardiogr. 2009; 10:165-193.
- Borlaug BA, Paulus WJ. Heart failure with preserved ejection fraction: pathophysiology, diagnosis, and treatment. Eur Heart J. 2011;32:670-679.
- Ponikowski P, Voors AA, Anker SD, Bueno H, Cleland JG, Coats AJ, Falk V, González-Juanatey JR, Harjola VP, Jankowska EA, Jessup M, Linde C, Nihoyannopoulos P, Parissis JT, Pieske B, Riley JP, Rosano GM, Ruilope LM, Ruschitzka F, Rutten FH, van der Meer P; Authors/Task Force Members. 2016 ESC Guidelines for the diagnosis and treatment of acute and chronic heart failure: The Task Force for the diagnosis and treatment of acute and chronic heart failure of the European Society of Cardiology (ESC) Developed with the special contribution of the Heart Failure Association (HFA) of the ESC. Eur Heart J. 2016;37:2129-2200.